Xavier Nassif M.D. PhD.
Course and current status
- Professor of Microbiology, University Paris Descartes, School of Medicine, Necker campus
- Head INSERM Unit 1002 : Pathogenesis of systemic infections
Scientific summary
Extra-cellular bacterial pathogens are the main cause of infections in developed countries and are often responsible for nosocomial infections. Paradoxically these bacteria are mostly commensal, and become invasive only in certain circumstances. Among the great variety of commensal bacteria that colonize a human, only few strains are able to disseminate. Furthermore some of these bacteria once septicemic can cross the blood-brain barrier and be responsible for meningitis.
Our goal is, using Neisseria meningitidis as a model, to identify the mechanisms by which (i) a bacteria can stop being a commensal and disseminate from its normal niche, and (ii) once it is septicemic how it can cross the blood brain barrier. N.meningitis is responsible for septicemia and meningitis after crossing of the blood brain barrier. Meningococcal meningitis remain a health threat in both developped and developping countries, and there is an urgent need for the development of a new vaccine strategy. Paradoxically, it is a commensal of human throat and colonizes a significant percentage of a population as healthy carrier. The reason why in some circumstances N.meningitidis can invade the bloodstream and become pathogenic remain unknown. Host factors are obviously important, however recently some clonal complexes have been shown to be more likely than others to be invasive.
We concentrate our work in two directions :
1. Identification of the bacterial attributes linked to invasiveness.
By comparative genomics, we have identified using a large collection of strains isolated from carriers and patients during the same period and in the same area that strains isolated from diseases were most likely to contain a prophage, designated Meningococcal Disease Associated (MDA) phage. We subsequently demonstrated that this phage belongs to the family of filamentous phage, like M13 and the CTX phage of Vibrio cholereae. Further work is ongoing in order to characterize the molecular mechanisms by which this phage increases invasiveness.
2. Identification of the interaction of N.meningitidis with the host cells in relation to the crossing of the blood-brain-barrier
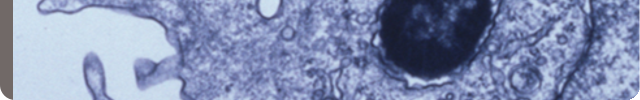
Our contribution has been to demonstrate that N. meningitidis cross this barrier by interacting directly with the endothelial cells of the blood brain barrier. We have shown, in collaboration with colleagues at the Institut Cochin (Sandrine Bourdoulous and Stefano Marullo) that during adhesion to host cells, N. meningitidis triggers a local remodeling of the eukaryotic cell surface resulting in a meshwork of cellular projections that can be found, in vitro and in vivo, inside and around microcolonies adhering to the cell surface. This signaling leads to the delocalization of junctional proteins at the site of bacterial cell interaction and the subsequent opening of the paracellular route. In addition we have shown that the type IV pili interact directly with the N-terminal portion of the beta2 adrenergic receptor to sigal to the cells. We are pursuing this work with the aim to identify the molecular interaction between the pili and the beta2 adrenergic receptor.
In addition during the course of this work, it became clear that N.meningitidis has to interact with two receptors one responsaible of the signaling (The beta2 adrenergic receptor) and one responsible for the bacterial adhesion. Work is currently ongoing to identify the adhesion receptor and its bacterial ligand.